Assessment, Optimisation and Shared Decision Making

CPOC Deputy Director
This is the last in the series of seven interventions to help people prepare for surgery. I have been warned that this is very difficult because it is all of medicine in one topic! So, here goes… There is more general detail in CPOC’s collaborative work about pre-operative assessment and optimisation. The principle is that assessment should go together with optimisation. This includes elective and emergency patients, although timescales differ, and some ‘emergency’ patients could go through a rapid planned pathway (such as ambulatory trauma lists).
Why does this matter?
A person’s functional status and their medical conditions have the biggest impact on how their anaesthetic or procedure might proceed, on how they will manage afterwards and on their risk of complications. Assessment should identify not only the severity of any issues, but also what might be improvable. These factors also alter the balance between benefits and risks. An assessment may identify factors warranting a further consultation for Shared Decision Making between the patient and a senior clinician and based on BRAN – the Benefits, Risks, Alternatives and No treatment options.
Numbers:
Some staff need to know the numbers to help their patients feel empowered to get these changes. For example:
- Around 12% of operations will have a complication.
- Complications are four times more likely for people living with frailty.
- Complications are at least four times more likely for people who are physically inactive.
- One study showed that being in the category of ASA 3 (with severe systemic disease) or higher was associated with 31% more complications, 2.5 days longer in intensive care and 24% longer length of stay compared with people in categories ASA 1 (no medical conditions) or ASA 2 (mild well-controlled medical conditions).
- Frail people over age 65 having emergency laparotomy surgery have 15.7% in-hospital mortality if no geriatrician is involved and 11.1% with geriatrician involvement. (This is 29% better, 3906 patients involved.)
- Preparation for surgery – principally exercise, smoking cessation, nutrition reduces risks by around 50%.
Assessment – and historical problems with timing and patient involvement:
For many years, pre-assessment has necessitated collating a considerable amount of documentation, and sometimes referring to other services (cardiology, diabetes, etc.) often with limited improvement. But there has been less focus on proactive optimisation of health. Unfortunately, the pre-assessment clinic appointment has often been very late in the process. The conversation has sometimes felt like a binary decision (operation or no operation) foisted onto a senior nurse or anaesthetist. There is an over-riding sense of passivity – with patients seldom involved in planning their care.
What should assessment look for to drive actions (especially optimisation)?
When undertaking assessments, we should be looking for aspects that are:
- stable but increase risk, or
- could be improved with medical intervention, and/or
- could be improved by the patient. NB It is safer to be active with a long-term condition than to be sedentary, or
- might need a change in process (eg requesting that a person with autism is first on the operating list), or
- might feed into an extra Shared Decision Making consultation – meaning a discussion between the patient and a senior clinician about whether an alternative operation or technique, or no treatment, might be preferable.
Timing of assessment - the potential of pre-screening
Pre-screening involves collecting proforma information early – at the time of a decision to operate. NHS England has recognised the benefits of this. Potential advantages of pre-screening:
- it allows time for patients to be supported to optimise their health and readiness for surgery (see the other 6 interventions to prepare for surgery)
- it requires someone to assess the information, perhaps allocating patients to “Red, Amber or Green” pathways. This helps:
- to decide whether early in-depth medical optimisation is required
- to streamline future appointments – allocating the seniority of clinician to complex patients
- It should allow capture of information, ideally electronically, that can populate the future pre-assessment process, to reduce the administrative burden.
How to assess functional capacity
- There are multiple specialist tools on Cardio-Pulmonary Exercise Testing.
- The simplest assessment is: “The inability to climb two flights of stairs or run a short distance indicates poor functional capacity.”
- Sit-To-Stand testing (how many times up from a chair in one minute) is helpful because it gives an activity to do later as well as providing an immediate assessment.
Functions of pre-assessment:
|
Medications:
Many people are on multiple medications for medical conditions. These often do more harm than good.
- There is a wider movement on de-prescribing.
- The planning of patient’s own medications around surgery are covered in: https://periop-handbook.ukclinicalpharmacy.org/
- Around 37% of elderly patients have problems with medication after discharge from hospital.
- Many people do not take their medication as prescribed, so coming into hospital may cause problems.
- Non-prescribed medication can cause problems.
- Some new weight loss medications can cause delayed stomach emptying, so the team need to be aware (eg to tilt the operating table).
Assessment and optimisation should include planning of medication.
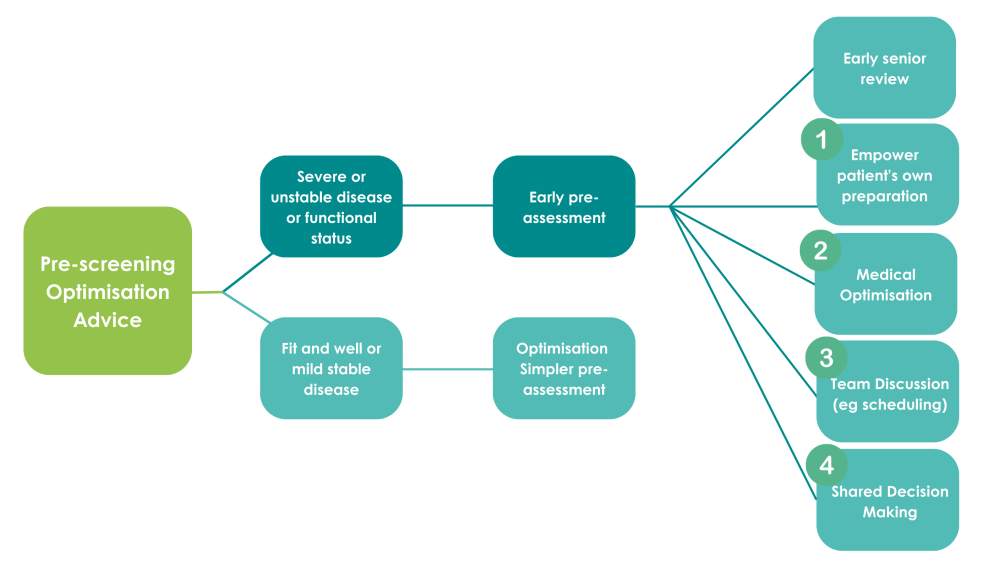
Figure 1: Assessment driving optimisation
Medical conditions:
There is huge range of medical conditions, some with more impact on anaesthesia or surgery than others. Heart and lung issues are most important (Table 1). When considering whether to refer, it is important to consider what might be changed (eg cardioversion, medication, etc).
The large reduction in complications with exercise, smoking cessation etc mean that patient preparation is far more effective than many medical interventions. Staff should consider learning about motivational interviewing, with features from ‘Making Every Contact Count’, and the practicalities that help patient preparation.
Table 1: Common issues that often require action during assessment, optimisation and shared decision making
|
|
Condition |
Why might this be important? |
Possible medical interventions? CPOC guidance available? |
Possible optimisation with patient-led interventions? |
Discussion about risk? |
|
Medications |
Diabetes medications |
Risk of low or high blood sugar |
Formal plan required |
See nutrition pages (NB risk of reversal of type 2 diabetes with low carb) |
|
|
“Blood thinners” |
Bleeding |
Follow guidance in https://periop-handbook.ukclinicalpharmacy.org/ |
Yes |
||
|
Inhalers |
Suggests airway obstruction is reversible |
|
|||
|
ALL other medications |
|
See guidance in https://periop-handbook.ukclinicalpharmacy.org/ |
|||
|
Common conditions that may be identified |
Hypertension |
Stroke if high BP |
Medication |
||
|
Pacemaker and Implantable defibrillator devices (ICD) |
|
Needs recent check |
|||
|
New arrythmias |
May be unstable |
Confirm with ECG |
|||
|
New heart valve problems |
Increases risk |
May need Echocardiogram |
|||
|
Obstructive Sleep Apnoea |
Increases risk |
https://www.cpoc.org.uk/guidelines-and-resources/guidelines/perioperative-management-osa-adults |
|||
|
Kidney problems |
Difficulty repairing tissue |
|
|||
|
Liver problems |
Difficulty forming proteins for healing and infection. |
|
|||
|
Diabetes |
Infections more likely |
https://www.cpoc.org.uk/guidelines-and-resources/guidelines/guideline-diabetes |
|||
|
Obesity |
Increased infection Increase operating time More anaesthetic issues |
|
|||
|
Anaemia |
Bleeding. Other complications. |
Assess/treat cause, eg Iron early https://cpoc.org.uk/guidelines-and-resources/guidelines/anaemia-perioperative-pathway |
|||
|
Frailty |
Large increase in risk. |
https://www.cpoc.org.uk/guidelines-and-resources/guidelines/perioperative-care-people-living-frailty |
|||
|
Mental health conditions |
May need individualised planning |
|
|||
|
Dental problems |
Loose crowns etc. |
Advise dental check |
|||
|
Life |
Low physical activity |
Increased complications |
See CPOC optimisation and patient pages |
||
|
Poor nutrition |
Other medical conditions
Some specialties or operations may have more specific requirements. The new Day Surgery Delivery Pack excludes very few patients from Day Surgery.
Minimum data
This is a personal plea. I find electronic notes often have multiple separate documents and it is difficult to find sufficient background information to make a good decision about surgery. Each patient’s notes should have, clearly accessible:
- A statement about the patient. This may be very short. For some patients it may be useful for a patient or carer to use the Alzheimer’s society template of “This is me” or other places have a “Care Passport”
- A list of medical conditions
- Medication
- Allergies
- A letter/explanation about why the operation is planned or being considered.
Risk
There are good websites about risk, such as www.sortsurgery.org. These should be used, especially with complex patients. This can determine
Shared Decision Making (SDM)
There is an excellent section of the CPOC website about Shared Decision Making. Each patient has different values. Many people would not want the risks of major complications and often the natural history of the condition is not clear – and operating may be worse than not operating. People with advanced age or multiple co-morbidities may feel that there is less to gain from having surgery. Shared Decision Making should be between the patient and a senior clinician who understands what each option involves. A good way to start is to consider BRAN – the Benefits, Risks and Alternatives of any treatment and the likely outcome with No treatment. There is a National institute for Health and Care Excellence (NICE) guideline NG197 mandating Shared Decision Making. This encourages “chunk and check” - giving patients information in manageable chunks and checking they understand (for example, using teach back). SDM is more important when there is equipoise between different options. When patients who are intending to have surgery have a Comprehensive Geriatric Assessment with a geriatric team, 14% of them decide against surgery. As an aside, I feel that the SDM discussion should include a commitment from the patient to prepare well for surgery.
Summary
Assessment should be early and should drive optimisation. Optimisation includes patient preparation and medical optimisation. Medications should be streamlined. Some aspects identified during the assessment will have an impact on risk and may warrant a further Shared Decision Making consultation with a senior clinician to determine whether the operation should go ahead.

