Diagnosing and treating tobacco dependency in acute care hospitals and the fundamental components of smoking cessation
Diagnosing and treating tobacco dependency in acute care hospitals and the fundamental components of smoking cessation
Prof Matthew Evison, Arran Woodhouse and Prof Scarlett McNally
Diagnosing and treating tobacco dependency in acute care hospitals – and the fundamental components of smoking cessation
Prof Matthew Evison, Arran Woodhouse and Prof Scarlett McNally
The Centre for Perioperative Care has new resources mainly focused on smoking cessation for outpatients. This builds on evidence from the World Health Organisation that smoking considerably increases the risk of complications of surgery and even a few weeks of smoking cessation before surgery significantly reduces this risk. Other organisations’ work is heavily focused on inpatients. Many components are fundamental and relevant to both inpatient and outpatient settings.
Two of us deliver tobacco dependency services across our hospital trusts in Manchester & London. The delivery of important new national frameworks for diagnosing and treating tobacco dependency in acute care hospitals needs multi-disciplinary support. Treating tobacco dependence is a major priority for the NHS and is an integral part of the NHS Long Term Plan. A key aspiration of the plan states that all people admitted to hospital who smoke will be offered NHS funded tobacco treatment services. There is a significant opportunity to diagnose and treat tobacco dependency in the hospital setting that falls on the shoulders of all hospital clinicians, supported by specialist practitioners. If, as a National Health Service, we could deliver this relatively simple & standardised intervention at scale and across all hospitals, the benefits in population health and health care utilisation would be unparallelled.
New Guidance and resources from two national organisations
In March 2024, the British Thoracic Society (BTS) published guidance on the medical management of tobacco dependency in hospitals. The introductory paragraph reads:
'Tobacco dependency is both the most common and deadliest co-morbidity a hospital clinician will encounter. The harms and costs of smoking and the substantial benefits of treating tobacco dependency during an acute hospital admission are well documented. This Clinical Statement has been developed to empower hospital clinicians with the knowledge, skills and confidence to provide expert, effective and evidence-based interventions for tobacco dependent patients as part of their admission. This will, in turn, ensure empathetic and meaningful interactions that are both professionally satisfying for the clinician and lifesaving for the patient, as well as ensuring excellence of care in tobacco dependency in line with NICE quality standards.'
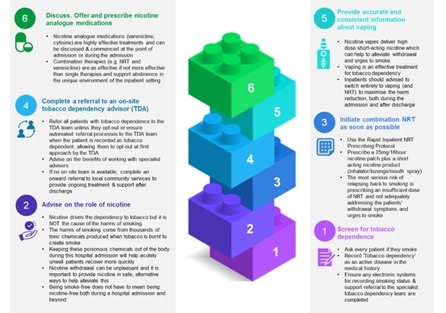
The BTS guidance includes a simple 'building block' framework that all clinicians could implement from the point of admission (Figure 1). Every clinician should be aware of the simple steps in the building block framework: 1. screen for tobacco dependence, 2. advise on the role of nicotine, 3. initiate a combination Nicotine Replacement Treatment (NRT) as soon as possible (typically 25mg/16hour nicotine patch plus a short acting nicotine product), 4. complete a referral to an on-site tobacco dependency advisor (TDA), 5. provide accurate and consistent information about vaping, and 6. discuss (offer and prescribe nicotine analogue medications).
To advise requires knowledge. The BTS explains that nicotine is highly addictive, but the harms of smoking occur due to the vehicle used for nicotine delivery, a tobacco-containing cigarette. The combustion of tobacco creates toxic chemicals and carcinogens which when inhaled in cigarette smoke, cause or exacerbate over one hundred different diseases. Nicotine triggers acetylcholine receptors in the brain and the consequent release of dopamine leads to effects for the user that include satiety and reward. People who smoke have a deeply engrained habit and become highly addicted to the rewarding effects of nicotine and can rapidly experience unpleasant withdrawal symptoms without it. Delivering nicotine replacement therapy (NRT) can help alleviate symptoms. NRT with behavioural support has the best chance of success for smoking cessation. The BTS guidance also states that vaping should be reduced gradually and not be used by non-smokers or people under age 18.
See Figure 1 below: Building blocks framework – British Thoracic Society, 2024
The BTS framework also includes supplementary resources, including:
- a scale for measuring tobacco dependency (based on number each day and how soon after waking the first cigarette is smoked – from within 5 minutes, 5–30, 30–31 and over 60 minutes) and number of years of smoking.
- the rationale and practicalities of using hand-held Carbon Monoxide monitors - raised CO readings usually indicate tobacco smoking and would normally be checked in the context of motivational support for people attempting or exploring a quit. (Exhaled CO levels in parts per million (ppm) of 5–9ppm is suggestive of ongoing exposure to smoked tobacco and 10ppm and above of ongoing smoking.)
- a separate evidence review with more detail about specific NRT products – for example a patient who has a cigarette within 30 minutes of waking probably needs 21mg/24 hour patch rather than 25mg/16 hours.
- advice on the practicalities of setting up a tobacco dependency service.
- This requires broad stakeholder engagement across IT system support, pharmacy & medicines management, Human Resources (HR), education & training, communications department & local authority / community pharmacy stop smoking services.
- At its head should be a critical leadership triumvirate of a clinical lead, an executive lead and project manager.
The National Centre for Smoking Cessation Training (NCSCT) also published in 2024 a series of resources and training packages that support the delivery of tobacco dependency treatment in Hospitals. This feels like a watershed moment in tobacco dependency to support all hospital clinicians taking proactive action to diagnose and treat this deadly disease.
The NCSCT provides Standard Treatment Plans (STPs) which are structured around the three Tobacco Dependence Treatment Care Bundles:
- Admission Care Bundle (starts with screening) - Identify, Advise, Treat, Refer, Record.
- Inpatient Care Bundle (tailoring medication, providing behavioural support and discharge planning)
- Post-Discharge Care Bundle (including follow up)
The NCSCT states:
A shared promise: We will never again refer to smoking as a ‘lifestyle choice’, or ‘bad habit’. Tobacco dependence is a powerful addiction and chronic relapsing clinical condition.
NCSCT has a useful guide to smoking cessation products and has free e-learning.
How to create or lead change in your service
The two of us who are clinicians involved in the production of these frameworks are really keen to try and maximise their impact. Considering the relevance to every medical and surgical specialty, we want to disseminate this work widely. We can offer a 'ready-made' grand round presentation, endorsed by the colleges that could be offered to all hospital trusts as well as bespoke events and communications.
The NHS is sometimes described as an anchor institution and has 1.7 million employees. The training “Making Every Contact Count” (MECC) is available free to all NHS staff. especially those in Bands 2–4 and/or those without a clinical qualification. It could be used to help other staff within the team, such as porters and receptionists to know how to communicate with patients about factors such as smoking. MECC helped promote routine screening for smoking and ‘Very Brief Advice’ (VBA) of ‘ask, advise, act’. MECC principles include listening for and amplifying “change talk” (such as why and how the patient may want to change) and acknowledging “sustain talk” that reinforce addictive behaviours. This is a chronic condition prone to relapse. There needs to be a repeated offer of support in many cases. NHS staff who manage to stop smoking have benefits across their community networks.
Connection with work ensuring NHS smokefree sites
Although all NHS sites have been smoke-free indoors since 2007 and outside since 2017, many places struggle with the reality of this. Many NHS sites experience difficulties trying to be ‘smoke-free’ and this is often related to NHS staff smoking. There is a pledge that NHS sites can sign. Medway hospital suggests five factors helped their success: 1. Providing support to quit for staff and visitors as well as patients, 2. Creating a team of stop smoking champions, 3. Strong leadership, 4. Communication (lots) and 5. Working closely with the estates team. Other sites have started with clear policies about smoking in work time needing to be off the premises or hospital site and out of uniform, backed up with training for managers, support for staff, e.g. to facilitate access to specialist support for tobacco dependence, work with communications (posters, letters to patients and instructions to visitors) and work with estates (types of bins and signage).
Information about oral tablets: Cytisine and Varenicline
Cytisine and Varenicline are medications that work on the nicotine receptor in the brain to create the same effects as nicotine but it also blocks nicotine from tobacco smoke having the same effect - taking away the rewarding experience of smoking and ‘breaking the addiction to tobacco’. Cytisine is now available for prescription in the UK for the first time ever. Varenicline is back available after a period where it was unavailable due an international recall (now available as generic Varenicline and not as 'Champix' the previous tradename of the Pfizer made medication). These are hugely effective medications and we must rapidly increase familiarity and confidence in prescribing these medications across the workforce.
- Cytisine is a 25-day course that de-escalates in dose over the 25 days from 6 tablets to 2 tablets. This might be useful for a rapid treatment course in a pre-operative setting.
- Varenicline is a 12-week course that increases in dose over the first week to a maintenance dose thereafter.
The Greater Manchester Make Smoking History team have created excellent educational seminars - on cytisine, varenicline and vaping — that can be downloaded from their website at https://makesmokinghistory.co.uk/partner-resources/smokefree-hospital-toolkit/ They are PowerPoint presentations with a voiceover so need to be listed to with the sound on!
Conclusion and call to arms!
2025 should be the year where all this comes together. Stopping smoking is the single best thing that any person can do for their future health. It is a tough addiction to stop. We know what works. The evidence exists. We should learn from success stories, and work with patients and staff. It is everyone’s business. We can do this!
Further resources:
- CPOC pages on stopping smoking (and halving complications of surgery) www.cpoc.org.uk/guidelines-resources-resources/stopping-smoking
- British Thoracic Society (BTS) 2024. www.brit-thoracic.org.uk/quality-improvement/clinical-statements/medical-management-of-inpatients-with-tobacco-dependency/
- The National Centre for Smoking Cessation Training (NCSCT), 2024. www.ncsct.co.uk/publications/category/inpatient-TDT-resources
- The Greater Manchester Make Smoking History team have created excellent educational seminars - on cytisine, varenicline and vaping — that can be downloaded from their website at https://makesmokinghistory.co.uk/partner-resources/smokefree-hospital-toolkit/ Listen with the sound on!
- Ash Action on Smoking and Health. Smokefree NHS Pledge https://ash.org.uk/resources/smokefree-nhs/the-nhs-smokefree-pledge
- Smokefree NHS tips for hospitals https://ukhsa.blog.gov.uk/2017/03/17/tobacco-free-nhs-troubleshooting-tips-for-hospitals/
- Medway smokefree hospital https://ukhsa.blog.gov.uk/2017/02/04/5-tips-on-how-to-go-smoke-free-from-medway-nhs-foundation-trust/
- Making Every Contact Count (MECC) training www.e-lfh.org.uk/programmes/making-every-contact-count/
About the authors:
Professor Matthew Evison
Consultant Chest Physician
Specialty Lead, Lung Cancer & Thoracic Surgery Directorate, Wythenshawe Hospital, Manchester University NHS Foundation Trust
Associate Medical Director, Greater Manchester Cancer
Clinical Lead, Make Smoking History, Greater Manchester Regional Tobacco Control Programme, NHS Greater Manchester
MASHC Honorary Clinical Chair, Faculty of Biology, Medicine & Health, University of Manchester
Arran Woodhouse
Lead Tobacco Dependence Specialist, King's College Hospital NHS Foundation Trust, London
Professor Scarlett McNally
Consultant Orthopaedic Surgeon, East Sussex Healthcare NHS Trust
Deputy Director, Centre for Perioperative Care www.cpoc.org.uk

