SipTilSend- The Story So Far

Dr Carol Gray is a consultant anaesthetist working in Tayside. Dr Gray went to medical school in Edinburgh and pursued her anaesthetic training in the West of Scotland. She is passionate about patient-centered care with a particular interest in perioperative improvement projects which focus on humanizing medicine. Dr Gray has been the clinical lead for emergency anesthesia and the pre-assessment service in Tayside. She has been involved in developing National recommendations for pre-assessment services and has implemented numerous service developments with the aim of improving the care and experience of emergency laparotomy patients.

Hannah Watson is a specialist nurse who works within Tayside. Hannah studied Adult Nursing at Dundee University and on qualifying, focused on her development within the surgical speciality wards. As well as SipTilSend, Hannah has been involved in several service development projects including Enhanced Recovery for All, which supports emergency and elective Colorectal and Upper GI patient groups. She has also been involved in quality improvement projects including those which have focused on person-centred care, clinical governance and the implementation of education to nursing staff.

I am a consultant anaesthetist and was a substantive consultant at Ninewells Hospital in Dundee from 1998 until October 2022. I am now a freelance anesthetist and continue to work with a wide range of patients and champion the benefits of @SipTilSend. I am co-authoring a Consensus Statement from the Association of Anaesthetists on the evolution of preoperative fluid fasting which will be published in 2025. With Carol Gray and Hannah Watson, I have established a SipTilSend national and international network to share experience and data.
SipTilSend was conceived and implemented by a small team of two anaesthetists, Dr Carol Gray and Dr Matthew Checketts, and specialist surgical nurse, Hannah Watson, at Ninewells Hospital in Dundee in 2021.
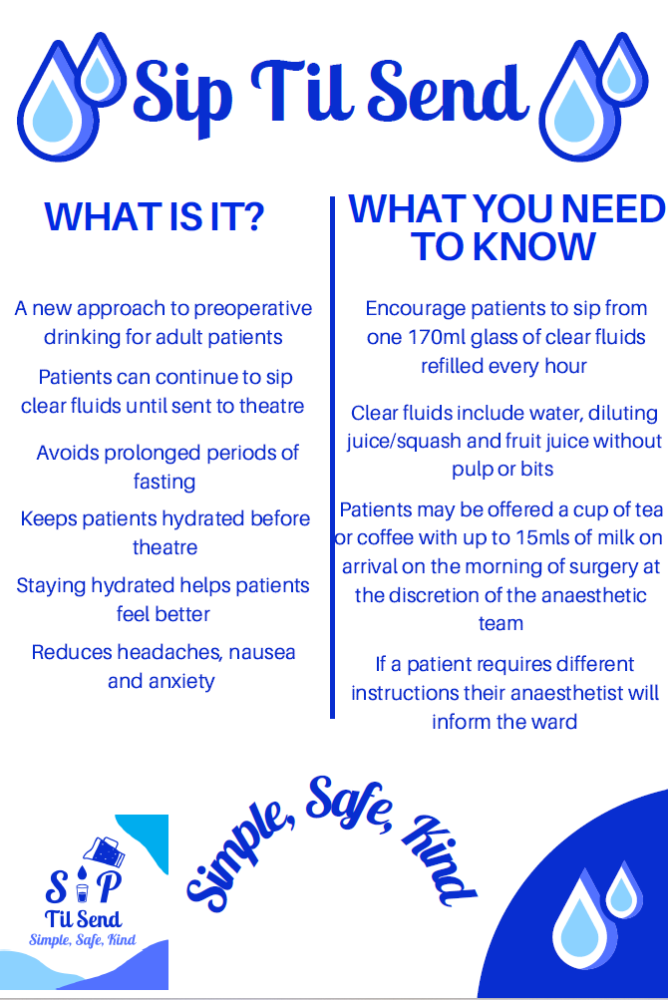
The concept of SipTilSend began following a local audit of fasting in unscheduled surgical patients, waiting for emergency theatres, which demonstrated a prolonged fluid fasting time of 7.5hours (median) with a range up to 22.5hrs. Previously, a number of differing approaches have been trialed to minimize fluid fasting but due to the unpredictable nature of theatre lists none of these have been successful. Cognoscente of the physiology of gastric emptying of clear fluids, we knew that the only way to reliably break this perennial problem of prolonged fasting was simply to allow patients to continue sipping water right up until they were sent for their procedures. And so, SipTilSend was born.
After presenting our initial audit findings to our local anesthetic department and receiving consensus support for the SipTilSend concept we followed up with a survey to the wider anaesthetic department asking ‘Would you be happy for your adult patients (with normal gastric emptying) to be allowed to sip up to 170 ml of clear fluid per hour until sent to theatre?’ 90% of anaesthetists agreed, giving us a mandate to take the idea though the relevant hospital governance processes.
The process of change then began which included a six-month education programme for everyone involved with patients undergoing procedures requiring sedation or anaesthesia. We created a team of SipTilSend champions from each ward area to support ongoing education and the implementation of the fasting changes. Our champions also managed the individual ward logistics of refilling patient glasses with water every hour. A number of information resources were developed and made available to all staff within the surgical wards. This approach ensured all members of the team knew and understood the changes prior to commencing. SipTilSend was launched as the default fluid fasting policy for all adult patients (both scheduled and unscheduled) across the three hospitals within our health board in December 2021. Subsequent audits demonstrated a reduction in median fluid fasting times from 7.5 hours to 17 minutes. Fasting time was defined as last drink until arrival at theatre reception. Not only have the fasting times improved dramatically, and reliably, but nursing staff on the wards have reported a better knowledge of fasting and highlighted the ease of following the simple concept. From the time of launch, we asked that any related adverse incidents be reported through our local hospital incident reporting systems which could then be reviewed.
After successful implementation of SipTilSend in NHS Tayside we shared the concept with the Scottish Hip Fracture Audit steering group where it was actively supported. Subsequently SipTilSend was rapidly adopted throughout the other Scottish NHS health boards.
The news of SipTilSend has travelled quickly and we have been approached by numerous hospitals throughout the UK and Internationally exploring how to adopt the changes to help keep patients comfortable and hydrated while waiting for surgery. So far, we have supported over 300 teams throughout the UK, Ireland and Australasia in their journey to implement SipTilSend through engagement sessions and sharing our implementation resources. It is clear that this simple concept has gained significant momentum in the anaesthetic community worldwide and crucially SipTilSend is improving the experience of patients waiting for surgery by reducing fluid deprivation.
CPOC has brought together SipTilSend Resources in one place.

